Hyperbaric oxygen therapy often sounds straightforward. You lie down, breathe pure oxygen, and let pressure do the rest. Reality looks more layered.
Time commitment varies by diagnosis. Session counts stretch from a handful to several dozen.
Pricing depends on where care happens, how it is billed, and whether insurance treats the indication as medically necessary. Anyone considering HBOT deserves a clear, grounded way to estimate both time and money before committing weeks or months of life to treatment.
What follows lays out session length, total course planning, and realistic cost expectations, all translated into plain language.
Let’s check the mechanics of how HBOT actually runs in clinical settings and how to read a quote without getting lost.
What Hyperbaric Oxygen Therapy Actually Involves

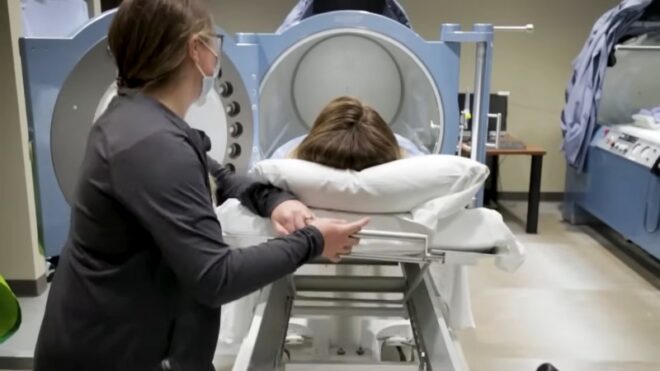
HBOT delivers 100% oxygen inside a sealed chamber pressurized above normal atmospheric levels. Most medical protocols operate around 2 to 3 atmospheres absolute.
Pressure at that level allows far more oxygen to dissolve into blood plasma, pushing oxygen deeper into tissues that struggle to heal under normal conditions.
Clinics rely on two main chamber designs. For readers looking to see how a modern oxygen chamber Los Angeles facility structures medical HBOT in practice, reviewing an actual treatment center can help ground expectations.
Monoplace Chambers
A monoplace chamber holds one person. It looks like a long, clear tube. Oxygen fills the chamber itself. Many outpatient centers rely on monoplace systems because they require less physical space and simpler logistics.
Multiplace Chambers
A multiplace chamber resembles a small room. Several patients sit or recline inside together. Oxygen reaches patients through masks or hoods. Hospitals and large wound centers often favor multiplace chambers for efficiency and staffing reasons.
Chamber type matters for experience and pricing. Multiplace chambers spread staffing and equipment costs across several patients at once. Monoplace sessions concentrate all costs into a single slot.
How Long One HBOT Session Really Takes
People often hear a single number quoted for session length. Actual appointment time stretches beyond oxygen breathing alone.
For many outpatient medical protocols, a typical session lands between 1 and 2 hours. Many sources cluster around 90 minutes to 2 hours for routine care.
Emergency protocols and select conditions may fall outside that window.
Some medical references note sessions as short as 45 minutes or as long as 300 minutes, depending on the indication. Diabetic foot ulcer protocols often fall between 45 and 120 minutes per day, repeated most weekdays over several weeks.
Oxygen Time Versus Door-To-Door Time
Clinics often advertise “oxygen time,” yet patients experience more than that. A realistic appointment includes preparation, pressure changes, and post-session checks.
A practical operational model breaks the visit into stages.
| Session component | What happens | Common time range |
| Check-in and safety prep | vitals, ear exam, clothing rules, item removal | 10 to 30 minutes |
| Pressurization | gradual pressure increase, ear pressure management | 5 to 15 minutes |
| Treatment at pressure | oxygen breathing with air breaks | 45 to 120 minutes |
| Depressurization and post-check | pressure return, vitals, ear check | 5 to 20 minutes |
Add those together and many centers block roughly 2.5 hours per appointment slot, even when oxygen exposure itself lasts about 90 minutes.
That distinction matters for work schedules, childcare, transportation, and fatigue planning.
How Many Sessions People Typically Need

Session count depends almost entirely on diagnosis and response to treatment.
Short-course indications exist. Carbon monoxide poisoning often resolves within a few treatments. Acute conditions aim to stabilize tissue quickly.
Chronic conditions tell a different story. Non-healing wounds, radiation injuries, and refractory bone infections require repetition. Tissue changes occur slowly, and protocols reflect that pace.
Common Planning Ranges Seen in Clinical Practice
Published treatment trend analyses offer useful planning ranges for cost and time estimation.
| Indication | Common session range |
| Diabetic foot ulcers | 30 to 40, sometimes up to 60 |
| Delayed radiation injury | 30 to 40, sometimes up to 60 |
| Refractory osteomyelitis | 30 to 40, sometimes up to 60 |
| Compromised grafts and flaps | around 20, sometimes up to 40 |
| Crush injury | fewer sessions than chronic wound care |
Numbers above represent planning ranges, not guarantees. Clinicians reassess progress throughout treatment. Lack of measurable improvement may shorten a course. Continued healing may extend it.
Insurance Rules Shape Real-World Course Length
Coverage policies influence session count as much as biology.
In the United States, Medicare covers HBOT only for a defined list of conditions. Diabetic wounds of the lower extremities fall under strict criteria.
Coverage requires documentation of severity and proof that standard wound care failed. Ongoing coverage also requires periodic re-evaluation, commonly every 30 days, with measurable improvement.
That structure explains why diabetic wound protocols often involve near-daily sessions for a month or longer. Coverage checkpoints dictate pacing.
HBOT Costs & What Patients Are Really Paying For
View this post on Instagram
Pricing confusion arises because multiple price layers coexist.
- Billed charges, often high and rarely paid in full
- Allowed or reimbursed amounts under insurance contracts
- Patient responsibility, including deductibles, copays, coinsurance, or self-pay rates
Most patients only experience the third layer, yet quotes often mention the first.
A Useful Baseline for Cost Planning
Medicare-based cost analyses provide a consistent anchor for planning, even for non-Medicare patients.
Published analyses estimate an average cost of around $595.86 per session in recent years, used for system-level planning. Separate payment updates break hospital outpatient billing into 30-minute segments, each reimbursed at a fixed rate. Multiply enough segments and the session total emerges.
Numbers above describe allowed system costs, not guaranteed patient bills. Still, they help frame scale.
What Drives Per-Session Cost
HBOT remains resource-intensive.
A detailed health economics report highlights major cost drivers.
- Personnel costs dominate, often accounting for roughly half or more of the total cost
- Chamber purchase and maintenance represent a major capital expense
- Oxygen and pressurized air contribute only a small fraction of the total cost
Chamber utilization changes everything. A multiplace chamber running at high occupancy spreads staff and equipment costs. A single-patient chamber concentrates them.
Turning a Per-Session Quote Into a Real Budget

To estimate personal cost, four inputs matter.
- Expected session count
- Treatment setting, hospital outpatient versus clinic-based center
- Coverage status, covered medical indication versus non-covered use
- Personal cost-sharing rules
A Planning Example Using Medicare-Style Math
Assume a 40-session course. Use an estimated $595.86 per session as a planning anchor.
- Total allowed system cost: about $23,834
- Coinsurance at 20%: about $119 per session
- Coinsurance total: roughly $4,767
Deductibles, supplemental coverage, and network status may alter that figure. The example above illustrates scale, not a promise.
Why Package Deals Raise Red Flags
Medical HBOT operates under strict safety rules, physician supervision, and documentation requirements. Coverage-based care rarely sells packages.
Wellness packages often bundle sessions at a flat cash price. Those offers may omit accreditation, physician oversight, or evidence-based indications. Lower price often reflects lower overhead and looser safety protocols, not clinical efficiency.
Insurance Coverage
@elixirhealthandwellness Hyperbaric Oxygen Therapy is a very popular insurance covered treatment in most of the world, except the United States. Here you are limited by: 1. What conditions are FDA approved (about 10 of them) 2. Will the hospital that has HBOT chambers take your insurance 3. Will a doctor write a script for you For centers like mine however…. A. You can sometimes use your HSA/FSA card (I accept both) B. Bill your insurance back depending why you’re coming in C. It’s sometimes CHEAPER to go to a Center like mine than what your insurance covered co-pay would even be The issue is that if the center owner is just jumping on a hot trend bandwagon, they may not be able to make the correct recommendation for you. I turn people towards other practitioners all the time for various reasons (I don’t have the correct equipment for their condition, I don’t know the research behind the protocol they want to do, they need to fix something in their lifestyle first). HBOT has hundreds of years of research behind it. Before you commit to something, make sure it personally applies to you! #mildhyperbaricchamber #hbot #hyperbaricchamber #wellnesscenter #lehighvalley ♬ original sound – Elixir Health and Wellness
Coverage depends on diagnosis, not desire.
Commonly Covered Medical Indications
Medicare and many private insurers cover HBOT for conditions such as:
- Acute carbon monoxide poisoning
- Decompression illness
- Gas embolism and gas gangrene
- Delayed radiation tissue injury
- Refractory osteomyelitis
- Compromised grafts and flaps
- Diabetic lower extremity wounds meeting strict criteria
- Selected crush injuries and acute ischemias
Coverage rules include documentation, re-evaluation intervals, and supervision requirements.
FDA Clearance Versus Insurance Coverage
FDA clearance governs device marketing, not payment. Chambers, cleared for certain serious conditions may still fall outside insurance coverage if documentation fails or criteria remain unmet.
Consumer guidance warns that many claims promoted outside clinical settings lack evidence. Conditions often advertised by wellness centers, including neurodegenerative disease, cancer, autism, or chronic infections, do not carry FDA clearance or insurance coverage.
Safety Rules That Affect Time and Cost

HBOT safety rules exist for good reason. Oxygen-rich environments increase fire risk.
Facilities enforce clothing restrictions, prohibit electronics, and limit skin products. Patients change into gowns. Staff perform ear checks before and after sessions.
Pressurization and depressurization occur gradually.
Federal safety communications highlight real injuries and deaths tied to improper chamber use, poor maintenance, or untrained staff. Accreditation and inspection matter. Skipping those safeguards lowers cost at the expense of risk.
Side Effects That Influence Total Burden
Most side effects remain mild and temporary, yet they affect planning.
- Ear or sinus discomfort
- Temporary vision changes
- Fatigue after sessions
Temporary nearsightedness appears in a significant minority of patients after extended daily courses. Vision often returns to baseline weeks after treatment ends.
For anyone who drives or works visually demanding jobs, that side effect carries indirect cost.
Rare serious events include lung injury or oxygen toxicity. Proper protocols minimize risk.
Avoiding Off-Label Sales Pitches
Cost discussions make sense only after confirming the indication.
Major medical centers caution against HBOT offered for unapproved uses outside accredited facilities. Federal consumer guidance echoes that warning, pointing to fires, injuries, and unsupported claims.
Accredited medical facilities, physician oversight, and evidence-based indications form the baseline. Anything less shifts risk onto the patient.
A Practical Way to Compare Providers
Step 1: Confirm Diagnosis and Indication
Ask the referring clinician to name the exact diagnosis being treated and whether HBOT qualifies as a covered medical service.
Step 2: Request a Written Course Estimate
Not a guarantee. A planning range.
- Expected session count
- Sessions per week
- Re-evaluation schedule
Step 3: Ask for an Itemized Estimate
Separate facility charges, professional supervision, and any wound care visits are commonly paired with HBOT.
Step 4: Verify Accreditation and Safety Standards
Accreditation signals staff training, maintenance standards, and emergency readiness.
Time Planning Examples
Short-Course Emergency Care
Acute poisoning or embolic events may require only a few sessions. Total cost reflects urgency and hospital resources more than repetition.
Chronic Wound Therapy
Diabetic foot ulcer protocols often run five days per week for weeks. Each visit occupies a substantial part of the day. Cumulative time commitment often surprises first-time patients more than cost.
Quick Reference Tables
Typical Session Length Ranges
| Source | Commonly reported session length |
| Outpatient medical centers | 1 to 2 hours |
| Chronic wound protocols | 45 to 120 minutes |
| Emergency protocols | highly variable |
Cost Drivers That Matter Most
| Cost driver | Practical meaning |
| Staffing | nurses, technicians, supervision |
| Equipment | chamber purchase and upkeep |
| Utilization | occupancy rate affects per-session cost |
| Coverage rules | documentation determines continuation |
Summary

Expect many outpatient HBOT sessions to run between 90 minutes and 2 hours door-to-door. Expect session counts to range from a handful for acute indications to 30 or more for chronic wounds and radiation injury.
Zinc oxide topicals are often used directly on wounds to support barrier protection and promote healing between therapy sessions.
Cost planning works best by separating system price from personal responsibility, anchoring estimates to session count, coverage status, and cost-sharing rules. Accreditation and safety practices deserve equal weight alongside price.





